Solving revenue capture for POCUS - The importance of workflow management
November 30, 2020
by Gus Iversen, Editor in Chief
HealthCare Business News sat down with Dr. John Hipskind, ultrasound GME director and ultrasound fellowship director at Kaweah Delta Medical Center to discuss the advantages of point-of-care ultrasound.
From reducing phantom scans, to easing credentialing and QA processes, and improving revenue overall, the technology has created tremendous opportunities for improvement at his facility.
HCB News: Tell us a bit about Kaweah Delta Medical Center. What kind of institution is it, and what’s the surrounding environment like?
Dr. Hipskind: We’re a 581-bed hybrid academic and Level III Trauma designated community hospital and Level III Trauma Center with 42 emergency department beds located in California’s Central Valley. We serve a catchment area of about half a million people, although the city we’re in, Visalia, has a population of around 125,000. In terms of annual volume, we were inching toward 100,000 patients early this year before COVID, but we’ll probably end the year around 75,000 visits
Our community has historically had poor access to care—we may not be a county hospital but we are definitely a safety net hospital. Years ago, we were finding it difficult to recruit enough physicians to serve our patients, as the Central Valley is quite a different place than your San Diego or L.A. In order to draw talented people here we started up a residence program in emergency and family medicine, launching the program 7 years ago. We now have 13 residents a year in that program, and more than 120 residents across all of Kaweah Delta’s departments. This past year we launched our own ultrasound fellowship program.
HCB News: With your residency program and trauma center status in mind, can you talk a bit about any specific point of care ultrasound (POCUS) workflow needs you have?
Dr. Hipskind: Well in short, we’re treating a large, often underserved patient population; we have a mission to train new physicians; and our role in the community means we need to secure enough revenue to maintain our sustainability.
Let’s start with the training aspect. We do about 400 point-of-care ultrasound scans every month in the ED, although things have of course fluctuated with COVID. To use those scans for training, though, we need an efficient way to mark interesting cases and to revisit residents’ scans to offer feedback on their techniques and interpretations. While all hospitals have PACS systems, those are often separate from the hospital email program and not automatically compliant with patient privacy regulations. Before our old system was sunsetted and we adopted Sonosite’s Synchronicity, it was nearly impossible to go back retrospectively and find a case a particular attending did with a particular resident—and if you did find it, you had to open your email program separately, still maintaining compliance, to share any tips. When there are barriers like those to timely, accurate feedback, it’s just not as beneficial to learners. You’re losing out on important recommendations and on effective changes they might have made.
The formal QA process governing residency was also extremely cumbersome with our old workflow system. When a resident sees any patient, they have to have an attending physician attest to being present for key components of the visit as well as all procedures—including ultrasounds. Another person then reviews the ultrasound scan for quality assurance, asking: Did the resident and the attending pick up all the findings? Could they have adjusted their technique a bit for a better scan? Removing barriers to locating scans and communicating feedback improves the learning curve of both residents and attendings.
For attendings, too, credentialing is a relevant issue: every two years they have to prove that they’ve accomplished a certain number of studies, for instance. With our old system this was extremely difficult to prove, and required Excel spreadsheets and a ton of painstaking labor. Now we can easily generate an administrative report simply by inputting the provider name, specific date range, and exam type. You can imagine how much better the staff responsible for that recredentialing feels about the new system.
HCB News: Are there any other QA or credentialing issues that fall to your point-of-care ultrasound workflow solution? Anything around your trauma center status, for instance?
Dr. Hipskind: Absolutely. It’s not exactly credentialing, but we do undergo an American College of Surgeons trauma accreditation . One thing they look at is what’s called an eFAST ultrasound, which is widely used to initially evaluate a critically ill patient. Emergency medicine physicians are obviously very facile with this—but the problem for us was that our surgeons were avoiding these scans. What we eventually learned was that they knew how to use the machine fine—it was the storage of the images, putting the images in PACS, and doing the QA that they found so difficult that they were avoiding it altogether. Our new system makes all of that intuitive and clear. Its ease of use is just amazing—which is important for evaluations, of course, but also because trauma centers depend on different specialists working closely together. Our patients deserve the best coordination, so if we can remove any unnecessary barriers, we should.
Let me share a brief story to illustrate how elegant our new Sonosite Synchronicity system is. Recently I was walking through how to do a scan on a stable trauma patient with a resident. He actually already knew how to do the scan, but he hadn’t yet stored the exam for QA and for the EMR, so I showed him how to do that on the new system. Two hours later we had a moderate trauma patient come in—and the resident said “Let me see if I can do this myself”—and on first pass he easily completed the documentation and actually made a really nice diagnosis. None of that would have ever happened with our old system.
HCB News: We understand you implemented Synchronicity during the pandemic - how was that experience?
Dr. Hipskind: Any Informatics install can be painful. With Covid-19 and the onsite implementation moved to on-line implementation support from Sonosite. The day we went live, we went live with Synchronicity and turned off the old system. We had a few issues but worked through them. Great communication with Sonosite support. We are months post the go-live and still have very good support.
HCB News: I hear you speaking a lot about the difficulties of the old workflow system but I’m wondering where the decision came from to replace it. Were issues of QA and barriers to communication the most important pain points for the decision-makers?
Dr. Hipskind: Well in our case we had a product that was going to be sunsetted, so we had to decide whether to upgrade with that company or move to a different workflow system altogether. Compounding some of the drawbacks I’ve discussed, we had always had a difficult time getting the IT support we needed—the sense I got was that the customer assistance wasn’t all that sophisticated. Frustrations like those might not rise to the awareness level of hospital administration, although they would certainly pay attention to something that’s making care more difficult, or impeding our training mission. I think the most compelling reasons we shifted to Synchronicity was its potential impact on patient care, reimbursement capture, and overall revenue—in particular through the reduction of “phantom scans.”
HCB News: What are those?
Dr. Hipskind: Those are scans that are performed, and which often drive clinical decisions, but are never archived or sent out for reimbursement due to gaps in documentation.
While it’s hard to measure a negative, I’ve seen the percentage of phantom scans estimated at something near 80% at some sites, and for us in the ED here it was about 25% before we switched systems.
HCB News: What exactly does the new system do to help you improve that revenue capture?
Dr. Hipskind: Well unlike many hospitals, we have always billed for ultrasounds. But there’s also always been a huge barrier to that process because the documentation requirements are so complex. Why was the screen done? What was seen? Was the image stored, and can you prove it hits all these other data points to qualify for reimbursement? Without all of those data points, the chart will be incomplete and you’ll be ineligible for payment. And these aren’t something you can memorize and jot down for later; the key to reimbursement, we’ve learned, is to have as many as possible of those questions asked and answered at the bedside.
Using badge scans and QR codes to populate certain necessary fields in a chart, we then work through the essential elements for reimbursement in a built-in worksheet we can complete during the patient visit. Our system then pushes those answers automatically to the EMR and PACS systems. The ease of locating past ultrasound scans via barcodes makes it far simpler to go back and add in information, too. The new system eliminated so many breaks in the chain of documentation—and it only takes one of those breaks to not be able to archive the images or lose a reimbursement.
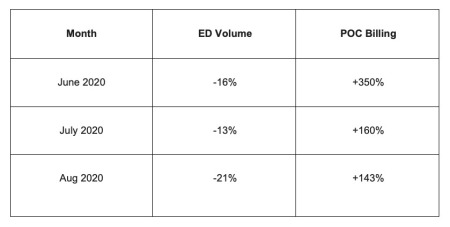
With the new system we’ve already gone from that 25% of uncaptured charges to something like 10%—and we’re only getting better as we continue adjusting our workflow. During this COVID period though our ED volume has decreased but our POCUS billing has increased because of Synchronicity. The attached is preliminary data and we expect to see even more improvements.
Actually, let me add another point about the revenue cycle for hospital leadership decision-makers. Reducing phantom scans obviously has a direct and quick ROI in our one department. But the revenue to the hospital overall, with its facility fees, is a multiple of the professional fees we’re capturing. That increase to the bottom line—from work that is already being performed—is all the more important with COVID driving down ER volumes.
From reducing phantom scans, to easing credentialing and QA processes, and improving revenue overall, the technology has created tremendous opportunities for improvement at his facility.
HCB News: Tell us a bit about Kaweah Delta Medical Center. What kind of institution is it, and what’s the surrounding environment like?
Dr. Hipskind: We’re a 581-bed hybrid academic and Level III Trauma designated community hospital and Level III Trauma Center with 42 emergency department beds located in California’s Central Valley. We serve a catchment area of about half a million people, although the city we’re in, Visalia, has a population of around 125,000. In terms of annual volume, we were inching toward 100,000 patients early this year before COVID, but we’ll probably end the year around 75,000 visits
Our community has historically had poor access to care—we may not be a county hospital but we are definitely a safety net hospital. Years ago, we were finding it difficult to recruit enough physicians to serve our patients, as the Central Valley is quite a different place than your San Diego or L.A. In order to draw talented people here we started up a residence program in emergency and family medicine, launching the program 7 years ago. We now have 13 residents a year in that program, and more than 120 residents across all of Kaweah Delta’s departments. This past year we launched our own ultrasound fellowship program.
HCB News: With your residency program and trauma center status in mind, can you talk a bit about any specific point of care ultrasound (POCUS) workflow needs you have?
Dr. Hipskind: Well in short, we’re treating a large, often underserved patient population; we have a mission to train new physicians; and our role in the community means we need to secure enough revenue to maintain our sustainability.
Let’s start with the training aspect. We do about 400 point-of-care ultrasound scans every month in the ED, although things have of course fluctuated with COVID. To use those scans for training, though, we need an efficient way to mark interesting cases and to revisit residents’ scans to offer feedback on their techniques and interpretations. While all hospitals have PACS systems, those are often separate from the hospital email program and not automatically compliant with patient privacy regulations. Before our old system was sunsetted and we adopted Sonosite’s Synchronicity, it was nearly impossible to go back retrospectively and find a case a particular attending did with a particular resident—and if you did find it, you had to open your email program separately, still maintaining compliance, to share any tips. When there are barriers like those to timely, accurate feedback, it’s just not as beneficial to learners. You’re losing out on important recommendations and on effective changes they might have made.
The formal QA process governing residency was also extremely cumbersome with our old workflow system. When a resident sees any patient, they have to have an attending physician attest to being present for key components of the visit as well as all procedures—including ultrasounds. Another person then reviews the ultrasound scan for quality assurance, asking: Did the resident and the attending pick up all the findings? Could they have adjusted their technique a bit for a better scan? Removing barriers to locating scans and communicating feedback improves the learning curve of both residents and attendings.
For attendings, too, credentialing is a relevant issue: every two years they have to prove that they’ve accomplished a certain number of studies, for instance. With our old system this was extremely difficult to prove, and required Excel spreadsheets and a ton of painstaking labor. Now we can easily generate an administrative report simply by inputting the provider name, specific date range, and exam type. You can imagine how much better the staff responsible for that recredentialing feels about the new system.
HCB News: Are there any other QA or credentialing issues that fall to your point-of-care ultrasound workflow solution? Anything around your trauma center status, for instance?
Dr. Hipskind: Absolutely. It’s not exactly credentialing, but we do undergo an American College of Surgeons trauma accreditation . One thing they look at is what’s called an eFAST ultrasound, which is widely used to initially evaluate a critically ill patient. Emergency medicine physicians are obviously very facile with this—but the problem for us was that our surgeons were avoiding these scans. What we eventually learned was that they knew how to use the machine fine—it was the storage of the images, putting the images in PACS, and doing the QA that they found so difficult that they were avoiding it altogether. Our new system makes all of that intuitive and clear. Its ease of use is just amazing—which is important for evaluations, of course, but also because trauma centers depend on different specialists working closely together. Our patients deserve the best coordination, so if we can remove any unnecessary barriers, we should.
Let me share a brief story to illustrate how elegant our new Sonosite Synchronicity system is. Recently I was walking through how to do a scan on a stable trauma patient with a resident. He actually already knew how to do the scan, but he hadn’t yet stored the exam for QA and for the EMR, so I showed him how to do that on the new system. Two hours later we had a moderate trauma patient come in—and the resident said “Let me see if I can do this myself”—and on first pass he easily completed the documentation and actually made a really nice diagnosis. None of that would have ever happened with our old system.
HCB News: We understand you implemented Synchronicity during the pandemic - how was that experience?
Dr. Hipskind: Any Informatics install can be painful. With Covid-19 and the onsite implementation moved to on-line implementation support from Sonosite. The day we went live, we went live with Synchronicity and turned off the old system. We had a few issues but worked through them. Great communication with Sonosite support. We are months post the go-live and still have very good support.
HCB News: I hear you speaking a lot about the difficulties of the old workflow system but I’m wondering where the decision came from to replace it. Were issues of QA and barriers to communication the most important pain points for the decision-makers?
Dr. Hipskind: Well in our case we had a product that was going to be sunsetted, so we had to decide whether to upgrade with that company or move to a different workflow system altogether. Compounding some of the drawbacks I’ve discussed, we had always had a difficult time getting the IT support we needed—the sense I got was that the customer assistance wasn’t all that sophisticated. Frustrations like those might not rise to the awareness level of hospital administration, although they would certainly pay attention to something that’s making care more difficult, or impeding our training mission. I think the most compelling reasons we shifted to Synchronicity was its potential impact on patient care, reimbursement capture, and overall revenue—in particular through the reduction of “phantom scans.”
HCB News: What are those?
Dr. Hipskind: Those are scans that are performed, and which often drive clinical decisions, but are never archived or sent out for reimbursement due to gaps in documentation.
While it’s hard to measure a negative, I’ve seen the percentage of phantom scans estimated at something near 80% at some sites, and for us in the ED here it was about 25% before we switched systems.
HCB News: What exactly does the new system do to help you improve that revenue capture?
Dr. Hipskind: Well unlike many hospitals, we have always billed for ultrasounds. But there’s also always been a huge barrier to that process because the documentation requirements are so complex. Why was the screen done? What was seen? Was the image stored, and can you prove it hits all these other data points to qualify for reimbursement? Without all of those data points, the chart will be incomplete and you’ll be ineligible for payment. And these aren’t something you can memorize and jot down for later; the key to reimbursement, we’ve learned, is to have as many as possible of those questions asked and answered at the bedside.
Using badge scans and QR codes to populate certain necessary fields in a chart, we then work through the essential elements for reimbursement in a built-in worksheet we can complete during the patient visit. Our system then pushes those answers automatically to the EMR and PACS systems. The ease of locating past ultrasound scans via barcodes makes it far simpler to go back and add in information, too. The new system eliminated so many breaks in the chain of documentation—and it only takes one of those breaks to not be able to archive the images or lose a reimbursement.
With the new system we’ve already gone from that 25% of uncaptured charges to something like 10%—and we’re only getting better as we continue adjusting our workflow. During this COVID period though our ED volume has decreased but our POCUS billing has increased because of Synchronicity. The attached is preliminary data and we expect to see even more improvements.
Actually, let me add another point about the revenue cycle for hospital leadership decision-makers. Reducing phantom scans obviously has a direct and quick ROI in our one department. But the revenue to the hospital overall, with its facility fees, is a multiple of the professional fees we’re capturing. That increase to the bottom line—from work that is already being performed—is all the more important with COVID driving down ER volumes.