RSNA opening session: A future beyond independent medical judgment
November 26, 2017
by John W. Mitchell, Senior Correspondent
CHICAGO -- Three speakers at the opening session of RSNA 2017 that opened in Chicago today described the rapidly evolving future of medicine and the role imaging is poised to play.
RSNA president Dr. Richard L. Ehman, led the discussion – “Is it Time it Reinvent Radiology?” - with a sober reminder. In the 1970’s if a car accident patient arrived in the ER with symptoms of a head injury but no fracture, the only way to determine if they had a brain bleed was for a surgeon to drill holes in the skull to check.
“This was the same procedure that was done 8,000 years ago in the Neolithic period. But that was state-of-the-art care not too long ago,” he told the capacity audience of 4,000 plus. “Imaging has changed medicine so profoundly that most physicians can’t imagine practicing without it.”
According to Ehman, rapid gains in imaging are characterized by team-led advances and practical applications of discoveries to solve an immediate medical problem. As an example, Ehman, who holds more than 30 MR patents, cited the invention of imaging in 1895.
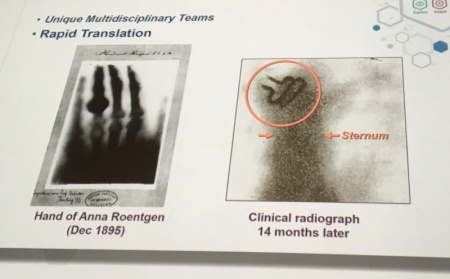
That was the year physicist Wilhelm Roentgen made an image of his wife’s hand using X-ray tubes. The first clinical application of the new technology occurred just 14 months later to find a buckle swallowed by a child. This despite the fact that a prominent surgeon of the day predicted X-ray had no useful medical application.
“Imaging relies on a use-inspired strategy with basic science as the most important starting point," said Ehman.
He also stressed the importance of patents as a measure of research success, as compared to the NIH emphasis on published articles. He noted a $33 return on investment in downstream economic patent inventions on every $6 NIH investment per $100 million. He also demonstrated a strong correlation between Nobel Prize recipients who were patent holders. Less than two percent of the NIH budget currently funds imaging research, Ehman said.
“[Radiologists] have to embrace disruption or be disrupted,” he cautioned. “We must guide the process rather than having it imposed upon us.”
The next two speakers fleshed out the details of how such a future is likely to evolve.
Dr. Roderic Pettigrew, founding director of the National Institute of Biomedical Imaging and Bioengineering at the NIH, and chair of a new Texas A&M program to integrate engineering into medicine, offered several examples of radiologists in their evolving role as biomedical data science experts.
He cited several current imaging research projects targeting diagnostics and therapies for several diseases. These include: much earlier diagnosis of Alzheimer’s disease; prostate “lumpectomy” to better target tumors; the first FDA-approved high speed, high-resolution 3-D Gd MR for improved diagnosis and treatment tracking of invasive ductal cancer, which increased interpretation by 50 percent and reduced missed cancers by 39 percent; and direct radiologist-to-patient counseling based on sequential chest CTs over time, to motivate patients to make lifestyle changes to reduce the risk of adverse cardiac events (in consultation with a cardiologist).
He also presented a video clip of four experts in three cities – London, Mumbai and Atlanta – working together virtually in real time through the use of avatars to diagnose the results of a patient colonoscopy conducted in London.
Such achievements, Pettigrew advocated, are all possible due to the rapidly evolving science of imaging deep-learning and artificial intelligence – or "radiomics." Radiomics is the emerging science where images are not merely pictures but data driven by the cross-disciplinary practices of radiology, pathology and genomics.
“Modern imaging is information science and will improve the value proposition of imaging,” said Pettigrew. “Tomorrow‘s radiologist will leverage AI.”
The final speaker at the opening session, Dr. Elias Zerhouni, a radiologist and biomedical engineer, is former Director of the National Institutes of Health and is currently president of global research and development at Sanofi.
“The leading edge of science … will be what is already here,” said Zerhouni. He explained that in 2003 he was asked to write a white paper about the future of imaging in 30 years. This seemed a monumental task that made him nervous, but when he looked back 30 years, such trends were already obvious and predictable.
He, too, said that imaging is more and more becoming interdisciplinary. He noted, for example, imaging recipients of Nobel awards have included 11 physicists, eight chemists and four physicians. He attributed this to the “tension between complexity and precision to unravel the … daunting complexity of biological systems in health and disease”. This, he added, is driven by the demand that precision medicine help control unsustainable health care costs.
According to Zerhouni, part of the solution is to eliminate the variation in the way radiologists practice medicine.
“We must improve our performance as a community … we need a revolution in medicine,” he told his colleagues.
Zerhouni said that in his career, he has noted that the way radiologists interpret findings is heterogeneous from one hospital to another. That has to change to a homogeneous system based on big data on the cloud, built and used by all radiologists to arrive at the same interpretations based on common AI standards. He, too, cited the concept of radiomics.
“We must take this direction very quickly,” Zerhouni said. “Future value (will be) who has the best reference data with most correlated molecular, cell and tissue (data). When you put this together, it allows you to compare your patient … to accurately track the evolution of diseases at the individual level.”
Radiologists, he said, have been the medical innovators in the past and they can do it again with a revolution of machine-augmented diagnostics.
“Ask not what radiology can do, but what we must do,” Zerhouni concluded.
RSNA president Dr. Richard L. Ehman, led the discussion – “Is it Time it Reinvent Radiology?” - with a sober reminder. In the 1970’s if a car accident patient arrived in the ER with symptoms of a head injury but no fracture, the only way to determine if they had a brain bleed was for a surgeon to drill holes in the skull to check.
“This was the same procedure that was done 8,000 years ago in the Neolithic period. But that was state-of-the-art care not too long ago,” he told the capacity audience of 4,000 plus. “Imaging has changed medicine so profoundly that most physicians can’t imagine practicing without it.”
According to Ehman, rapid gains in imaging are characterized by team-led advances and practical applications of discoveries to solve an immediate medical problem. As an example, Ehman, who holds more than 30 MR patents, cited the invention of imaging in 1895.
That was the year physicist Wilhelm Roentgen made an image of his wife’s hand using X-ray tubes. The first clinical application of the new technology occurred just 14 months later to find a buckle swallowed by a child. This despite the fact that a prominent surgeon of the day predicted X-ray had no useful medical application.
“Imaging relies on a use-inspired strategy with basic science as the most important starting point," said Ehman.
He also stressed the importance of patents as a measure of research success, as compared to the NIH emphasis on published articles. He noted a $33 return on investment in downstream economic patent inventions on every $6 NIH investment per $100 million. He also demonstrated a strong correlation between Nobel Prize recipients who were patent holders. Less than two percent of the NIH budget currently funds imaging research, Ehman said.
“[Radiologists] have to embrace disruption or be disrupted,” he cautioned. “We must guide the process rather than having it imposed upon us.”
The next two speakers fleshed out the details of how such a future is likely to evolve.
Dr. Roderic Pettigrew, founding director of the National Institute of Biomedical Imaging and Bioengineering at the NIH, and chair of a new Texas A&M program to integrate engineering into medicine, offered several examples of radiologists in their evolving role as biomedical data science experts.
He cited several current imaging research projects targeting diagnostics and therapies for several diseases. These include: much earlier diagnosis of Alzheimer’s disease; prostate “lumpectomy” to better target tumors; the first FDA-approved high speed, high-resolution 3-D Gd MR for improved diagnosis and treatment tracking of invasive ductal cancer, which increased interpretation by 50 percent and reduced missed cancers by 39 percent; and direct radiologist-to-patient counseling based on sequential chest CTs over time, to motivate patients to make lifestyle changes to reduce the risk of adverse cardiac events (in consultation with a cardiologist).
He also presented a video clip of four experts in three cities – London, Mumbai and Atlanta – working together virtually in real time through the use of avatars to diagnose the results of a patient colonoscopy conducted in London.
Such achievements, Pettigrew advocated, are all possible due to the rapidly evolving science of imaging deep-learning and artificial intelligence – or "radiomics." Radiomics is the emerging science where images are not merely pictures but data driven by the cross-disciplinary practices of radiology, pathology and genomics.
“Modern imaging is information science and will improve the value proposition of imaging,” said Pettigrew. “Tomorrow‘s radiologist will leverage AI.”
The final speaker at the opening session, Dr. Elias Zerhouni, a radiologist and biomedical engineer, is former Director of the National Institutes of Health and is currently president of global research and development at Sanofi.
“The leading edge of science … will be what is already here,” said Zerhouni. He explained that in 2003 he was asked to write a white paper about the future of imaging in 30 years. This seemed a monumental task that made him nervous, but when he looked back 30 years, such trends were already obvious and predictable.
He, too, said that imaging is more and more becoming interdisciplinary. He noted, for example, imaging recipients of Nobel awards have included 11 physicists, eight chemists and four physicians. He attributed this to the “tension between complexity and precision to unravel the … daunting complexity of biological systems in health and disease”. This, he added, is driven by the demand that precision medicine help control unsustainable health care costs.
According to Zerhouni, part of the solution is to eliminate the variation in the way radiologists practice medicine.
“We must improve our performance as a community … we need a revolution in medicine,” he told his colleagues.
Zerhouni said that in his career, he has noted that the way radiologists interpret findings is heterogeneous from one hospital to another. That has to change to a homogeneous system based on big data on the cloud, built and used by all radiologists to arrive at the same interpretations based on common AI standards. He, too, cited the concept of radiomics.
“We must take this direction very quickly,” Zerhouni said. “Future value (will be) who has the best reference data with most correlated molecular, cell and tissue (data). When you put this together, it allows you to compare your patient … to accurately track the evolution of diseases at the individual level.”
Radiologists, he said, have been the medical innovators in the past and they can do it again with a revolution of machine-augmented diagnostics.
“Ask not what radiology can do, but what we must do,” Zerhouni concluded.